 Radical Prostatectomy
Radical Prostatectomy
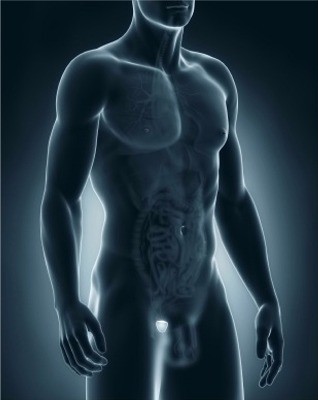
A radical prostatectomy is the surgical removal of your prostate gland, to cure prostate cancer that has not spread outside the prostate.
This prostate surgery is performed under a combined general and spinal anaesthetic and involves removing the entire prostate gland, seminal vesicles (glands that produce semen) and other tissue that may contain cancer cells – possibly nearby blood vessels, nerves and fat.
Once they have been removed, the urethra (the tube that carries urine through the penis and out of the body) is re-attached to the bladder.
A radical prostatectomy can be performed using laparoscopic or open surgery. In traditional open surgery a single incision of about 10-15cm is made in the abdomen.
Laparoscopic or keyhole surgery is carried out using five small incisions rather than one large one. Special endoscopes are inserted into these, one to transmit pictures of the inside of the body to a computer screen, the others carrying surgical instruments used during the procedure.
Prostate surgery is just one treatment option. Other procedures may be more appropriate for your grade and stage of cancer, or might be used in conjunction with radical prostatectomy. [Read More at Prostate Cancer]
Erectile dysfunction
Some form of erectile dysfunction is inevitable following a prostatectomy. For some men, this gradually improves, but around half of men will have long-term problems.
However our surgeons can, under certain circumstances, try to preserve the neurovascular bundles – nerves and blood vessels that are attached to the prostate and help produce normal erections.
Up to 80% of men below 60 years of age who previously had good erections recover erectile function after surgery where the neurovascular bundles are preserved, but it can take up to 2 years.
Nerve preservation can only be done if there is no clear sign of cancer on the outside of the prostate, especially close to the neurovascular bundles, and there is the possibility that preserving the neurovascular bundles could leave some cancer behind.
If you have problems getting an erection before surgery, you are more likely to have problems after prostate surgery. Other risk factors that will effect erections include high blood pressure, diabetes and smoking.
Whilst orgasm may eventually be possible, you will no longer ejaculate any semen, and will be infertile. You may want to ask your specialist about storing a sperm sample before prostate surgery, so it can be used later for IVF (in vitro fertilisation).
After surgery, you may need to use a catheter (a flexible tube that you place into your bladder) to remove urine from your bladder while your urethra recovers. Many men experience pain while urinating for several weeks after the operation.
Incontinence
Some men have problems with incontinence, from leaking small drops of urine to larger amounts that require pads. This usually clears up within three to six months of the operation for most men, but some will have long-term problems.
Strengthening the pelvic floor muscles before and after the operation can help in the long term, and our specialist physiotherapist will teach you pelvic floor exercises.
Pelvic floor exercises
Pelvic floor exercises are proven to improve incontinence in men after surgery to remove the prostate gland.
They strengthen and tone the muscles that support the pelvic organs and are an essential part of improving incontinence and preventing it from worsening. Pelvic floor exercises do require commitment and regular practice, and learning the correct technique is also very important. Only 10-15% of patients who attend continence clinics and carry out the exercises have to be referred for further surgery.
If you can contract your pelvic floor muscles, you will be taught certain exercises involving muscle contractions to do at least three times a day for at least three months. If the exercises work for you they can be continued indefinitely.
Biofeedback
If you find it difficult to locate your pelvic floor muscles or are unsure if you’re doing pelvic muscle exercises correctly, Biofeedback therapy can help you learn to control them properly.
Biofeedback therapy uses computer graphs and audible tones to show you the muscles you are exercising. It also allows your therapist to measure your muscle strength and tailor your exercise programme to suit you.
At Somerset Urology our continence advisers and incontinence physiotherapists are particularly experienced at teaching pelvic floor exercises to strengthen muscles that have become weak.
